Allergies or COVID? Here’s How to Tell the Difference
Key takeaways:
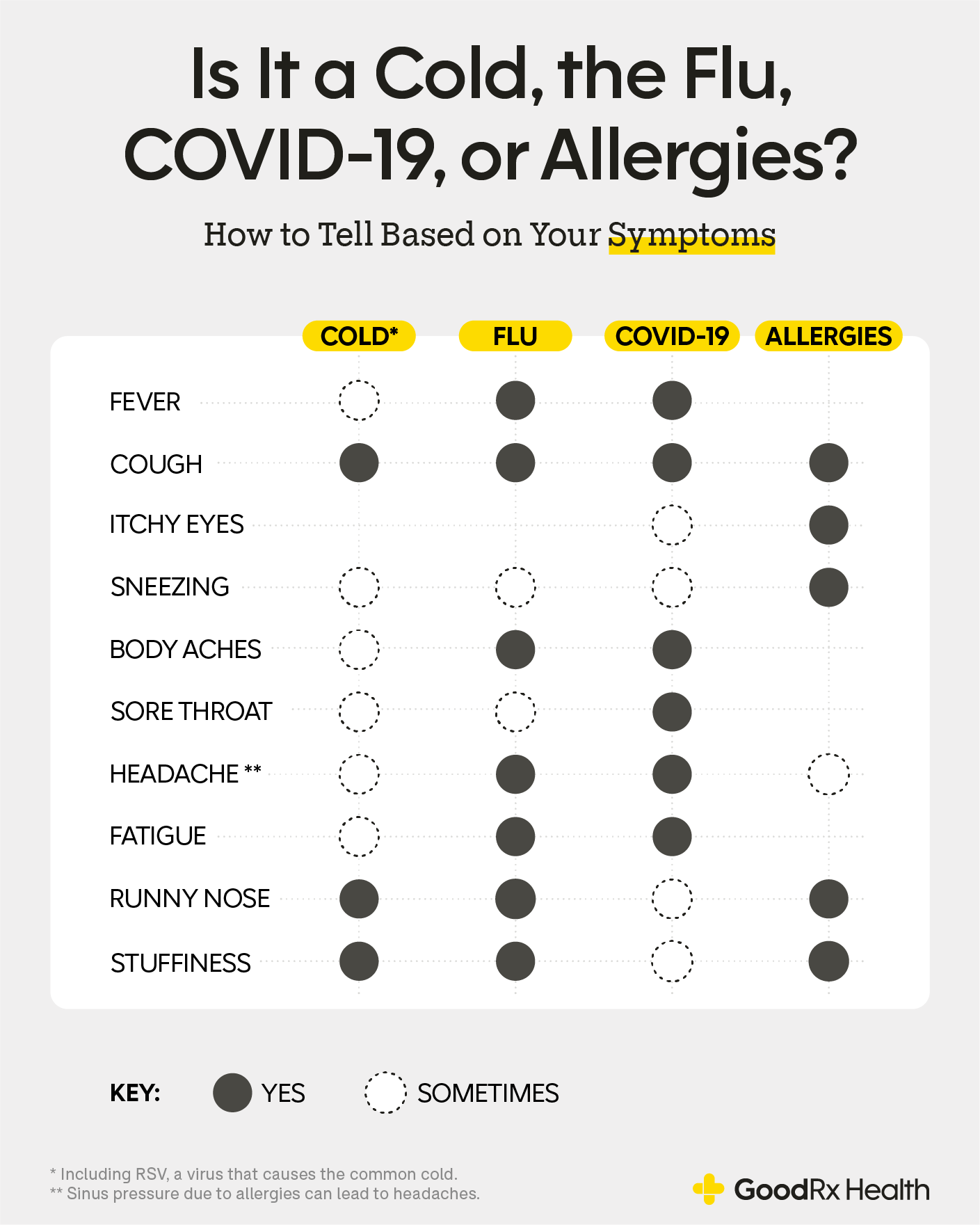
Allergies and COVID-19 can cause similar respiratory symptoms, making it difficult to tell them apart.
The main difference between allergies and a COVID infection is that COVID can cause fever, whereas allergies do not.
The only way to tell for sure whether your symptoms are from a COVID infection rather than allergies is a positive COVID test.

If you have seasonal allergies, you know how uncomfortable it can be when your symptoms flare up. Allergies can cause a stuffy nose, cough, and fatigue. But these symptoms are very similar to those of a COVID-19 infection. So it’s common to wonder whether your symptoms are due to COVID or allergies.
Let’s take a closer look at how you can tell the difference between COVID versus allergy symptoms — and what you can do to feel better.
COVID-19 vs. allergies
Seasonal allergies, also called “hay fever,” flare in the spring and fall. Perennial allergies (such as those to dust and mold) are around all year. The tricky thing is that allergies can behave like COVID.
Both COVID and allergies can cause symptoms like:
Runny nose
Nasal congestion
Sore throat
Irritated eyes
Fatigue
Differences between COVID symptoms and allergies
The major differences between allergy and COVID symptoms are:
Fever: Allergies shouldn’t cause any increase in temperature. If you detect a fever of 100°F or higher, this points to an infection and not allergies. Not everyone with COVID gets a fever, but it occurs in many people with the infection.
Itching: Itching is a characteristic symptom of allergies but not COVID. Allergies can cause itchy eyes, nose, throat, and skin.
Length of symptoms: Allergy symptoms last much longer than viral infections. COVID symptoms usually clear up within 1 to 2 weeks. Pollen seasons can last for a couple of months, and perennial allergies are around all year.
COVID can also cause symptoms that affect other organs. These are uncommon with allergies. Examples include:
Chest tightness, shortness of breath, cough, or wheeze
Loss of smell and taste
Muscle and joint pain
Headache
Nausea, vomiting, and diarrhea
Skin symptoms, such as rashes and other skin changes
Is it allergies or COVID?
Sometimes it can be hard to tell the difference between allergies and COVID. This is especially true when symptoms are just starting. But subtle clues, like fever or symptoms beyond the upper respiratory system, can help tell them apart.
If you know you’ve been exposed to COVID, it’s best to be safe and take a COVID test. And follow current CDC guidelines after a known exposure, even if you have a history of seasonal allergies.
Sore throat: Allergies or COVID?
Sore throat is a common symptom of COVID. It may occur along with other symptoms, such as fever and congestion, or it may be the first symptom to develop. One small study suggests that the Omicron variant may first infect the throat instead of the nose.
Many people with allergies also complain of a sore throat due to postnasal drainage — when mucus drips down the back of the throat. This can be worse in the early morning after lying down at night.
Sore throats from allergies usually occur with other allergy symptoms and don’t occur alone. In other words, your sore throat could be due to either COVID or allergies. Your other symptoms can help point to a cause, but the only way to know for sure is to take a COVID test.
Cough: Allergies or COVID?
Both COVID and allergies can make you cough. With allergies, increased mucus and postnasal drainage that irritates the throat also cause coughing. It can also feel like a tickle or itch in your throat. Allergies can also cause chest symptoms if you have allergic asthma.
On the other hand, a cough due to COVID develops when the lungs are affected. The cough is usually dry, meaning that it doesn’t produce any mucus or phlegm. You may have other chest symptoms with your cough, such as shortness of breath, chest discomfort, and wheeze.
Hoarse voice: Allergies or COVID?
Both COVID and allergies can cause voice changes like hoarseness. Hoarseness can happen with allergies due to irritation from postnasal drip. The drainage and mucus can lead to inflammation in the throat and voice changes.
It’s also fairly common to have a hoarse voice with COVID. In one study looking at over 13,000 people, about 1 in 4 people with COVID reported voice changes. And some even reported long-lasting changes.
Sinus pressure: Allergies or COVID?
Sinus pressure can occur with both allergies and COVID. Sinus pressure is a familiar hallmark of allergy season, and it’s pretty common with COVID, too.
There’s not a lot of data about sinus pressure as a symptom of COVID infection. But one small study found that about half of people with COVID infection reported sinus inflammation.
See your healthcare provider if allergy medications don’t relieve your sinus pressure, or if you develop a fever. Allergies and viral infections (like COVID) can lead to sinus infections, which may need antibiotics.
Headache: Allergies or COVID?
A headache can happen with both allergies and COVID. Headache is one of the most common symptoms of COVID infection — second only to respiratory symptoms. And sinus pressure with allergies can often trigger a sinus headache as well.
If you have a headache and you’re concerned about COVID, a quick COVID test can point you in the right direction. Always let your healthcare provider know if you have unexplained headaches.
Can you have COVID and allergies at the same time?
Yes, you can have COVID and allergies at the same time. Interestingly, people with allergies may be at lower risk of getting COVID. This may be because allergic airways have a reduced expression of ACE2, the receptor for COVID.
In another study, nasal steroid sprays — a common treatment for allergies — seemed to decrease the severity of COVID.
What to do if you aren’t sure it’s allergies or COVID
A good way to tell the difference between COVID and allergies is checking your temperature at home. If you have a fever, then you most likely have some kind of infection.
And consider your response to allergy treatments. You can manage most of your allergy symptoms with over-the-counter antihistamines and nasal steroid sprays. If your symptoms go away with these medications, then you probably do not have a serious illness.
When should you get a COVID test?
If you aren’t sure what’s causing your symptoms, your provider can help figure it out. Consider a telemedicine visit so that you can speak with your provider without leaving your house.
While waiting to talk with your provider, it’s better to err on the side of caution. That means you should isolate yourself, sanitize surfaces, and wear a mask. And avoid social settings until you’re sure that it’s only allergies.
At the end of the day, only a formal COVID test can definitively tell the difference between COVID and allergies. Getting tested is important to prevent the spread of COVID.
There are two main types of tests to see if you’re infected with COVID. Both are done by swabbing the nose and/or throat for the virus:
Rapid tests: You can do rapid tests at home or testing sites. You’ll get results within 15 minutes. Rapid tests are convenient but have a higher chance of missing an active infection.
Laboratory tests (PCR tests): Results take longer, but they’re the most reliable at identifying an infection.
Here’s a helpful tool to find a testing site close to you.
The bottom line
COVID-19 can be hard to tell apart from other conditions with similar symptoms, like allergies. There are some subtle differences, but fever is the key symptom that helps to tell the difference between COVID and allergies. If you’re concerned that you may have COVID, talk with your provider about your symptoms and get tested. It’s always best to be extra cautious and isolate yourself until you know for sure.
References
Centers for Disease Control and Prevention. (2022). What to do if you were exposed to COVID-19.
Centers for Disease Control and Prevention. (2023). COVID-19 testing: What you need to know.
Genovese, G., et al. (2021). Skin manifestations associated with COVID-19: Current knowledge and future perspectives. Dermatology.
Holt, H., et al. (2022). Risk factors for developing COVID-19: A population-based longitudinal study (COVIDENCE UK). Thorax.
Jackson, D. J., et al. (2020). Association of respiratory allergy, asthma, and expression of the SARS-CoV-2 receptor ACE2. The Journal of Allergy and Clinical Immunology.
Lin, C. W., et al. (2023). COVID-related dysphonia and persistent long-COVID voice sequelae: A systematic review and meta-analysis. American Journal of Otolaryngology.
Marais, G., et al. (2022). Improved oral detection is a characteristic of Omicron infection and has implications for clinical sampling and tissue tropism. Journal of Clinical Virology.
Strauss, R., et al. (2021). Intranasal corticosteroids are associated with better outcomes in coronavirus disease 2019. The Journal of Allergy and Clinical Immunology.
Togha, M., et al. (2022). A review on headaches due to COVID-19 infection. Frontiers in Neurology.
U.S. Department of Health and Human Services. (2023). Coronavirus (COVID-19) testing.
Williams, R. K., et al. (2022). Whole-organ transdermal photobiomodulation (PBM) of COVID-19: A 50-patient case study. Journal of Biophotonics.